If you’re caring for someone with dementia, you’ve probably noticed how sleep problems can turn nights into a struggle—for both of you. Sleep issues in dementia patients aren’t just about feeling tired; they can worsen confusion, increase agitation, and affect overall health.
You might wonder how to help your loved one rest better without constant interruptions or distress. This article will guide you through simple, effective ways to manage sleep difficulties in dementia, helping you create peaceful nights and brighter days. Keep reading to discover practical tips that can make a real difference for you and your loved one.
Credit: www.aging-us.com
Sleep Problems In Dementia
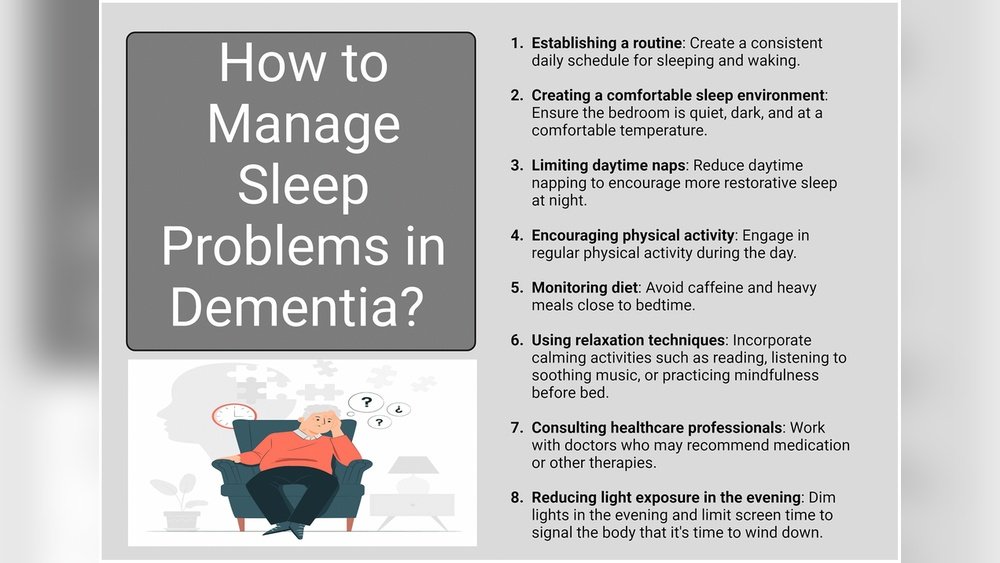
Sleep problems are common in people with dementia. These issues affect both the patient and their caregivers. Understanding these problems helps manage them better. Sleep changes vary with dementia stages. Some symptoms can be challenging at night. Recognizing these patterns improves care and comfort.
Common Sleep Issues
Dementia often causes trouble falling asleep. Patients may wake up many times during the night. Daytime sleepiness or napping is frequent. Nighttime wandering and confusion are also common. These problems disrupt normal sleep patterns. Caregivers face challenges helping loved ones rest well.
Sleep Changes By Dementia Stage
In early stages, sleep may be mostly normal. Mild changes like restless nights might appear. Middle stages bring more sleep disturbances. Patients may have trouble staying asleep. Daytime drowsiness increases, affecting daily activity. Late stages often reverse sleep cycles. Patients may stay awake at night and sleep during the day. This stage needs more care and attention.
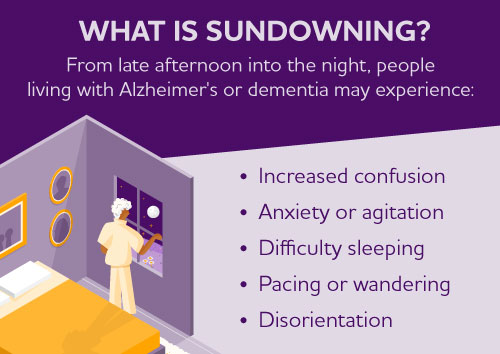
Sundowning And Nighttime Agitation
Sundowning means increased confusion in late afternoon or evening. It causes restlessness and agitation. Patients may pace, shout, or become anxious. This behavior makes nighttime care difficult. Identifying sundowning helps find ways to calm patients. Creating a quiet, safe environment reduces agitation. Consistent routines and soft lighting aid relaxation.
Credit: www.alz.org
Triggers For Sleep Disturbances
Sleep disturbances are common in dementia patients. Understanding triggers helps manage these issues better. Several factors can disrupt their sleep patterns. Identifying these causes allows caregivers to create a calming sleep routine.
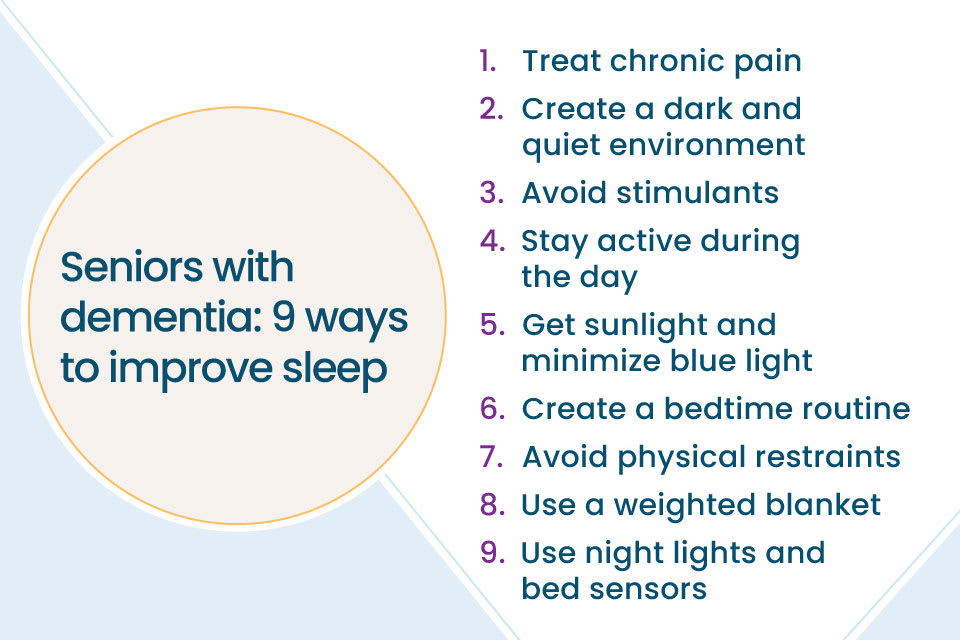
Unmet Physical Needs
Physical discomfort often disrupts sleep in dementia patients. Hunger or thirst can cause restlessness. Pain from arthritis or other conditions may wake them. Sometimes, needing to use the bathroom interrupts sleep. Simple checks for these needs can improve restfulness.
Emotional Discomfort
Emotions affect sleep quality significantly. Anxiety or fear can keep a person awake. Confusion about surroundings may cause distress at night. Loneliness can also lead to restless nights. Providing comfort and reassurance helps ease these feelings.
Environmental Factors
The bedroom environment plays a vital role in sleep. Noise from outside or inside can wake patients. Bright lights may confuse the body’s natural clock. An uncomfortable bed or room temperature disturbs rest. Creating a quiet, dark, and cozy space supports better sleep.
Creating A Restful Environment
Creating a restful environment is key to managing sleep issues in dementia patients. A calm, peaceful bedroom helps reduce confusion and restlessness. Simple changes in the bedroom can make a big difference in sleep quality. Focus on comfort and minimal distractions to promote better rest. This section covers three important ways to create a restful space.
Optimizing Bedroom Settings
Choose a quiet, familiar room for sleep. Keep the bedroom tidy and free of clutter. Use simple, soft bedding that feels good on the skin. Position the bed so natural light can enter during the day. Avoid busy patterns on walls or bed linens. These can cause confusion or overstimulation. Make sure the mattress supports comfort and body alignment. A good bed reduces tossing and turning. Add personal items that bring calm, like photos or a favorite blanket.
Reducing Noise And Light
Lower noise levels to help the patient relax. Use soft background sounds like white noise or gentle music. Avoid sudden or loud noises that may cause distress. Limit light exposure in the evening to signal bedtime. Use blackout curtains to block streetlights or early morning sun. Turn off electronic screens at least an hour before sleep. Dim lamps or nightlights create a soothing atmosphere. Too much light can confuse the body’s sleep signals. Keep the room dark enough for deep rest.
Maintaining Comfortable Temperature
Set the bedroom temperature between 60 and 67 degrees Fahrenheit. This range suits most people and helps sleep quality. Avoid extreme heat or cold that can disrupt sleep. Use fans or heaters carefully to maintain steady warmth. Dress the patient in breathable, comfortable clothing. Layer bedding to adjust warmth as needed. Check the room temperature regularly and adjust for seasons. A stable temperature reduces night waking and discomfort. Comfort supports longer and more restful sleep periods.
Establishing Healthy Routines
Establishing healthy routines plays a key role in managing sleep issues in dementia patients. A stable routine helps reduce confusion and anxiety. It supports the body’s internal clock, making sleep more natural and restful. Caregivers can create a calm and predictable environment by setting daily habits. This improves the quality of life for both the patient and the caregiver.
Consistent Sleep Schedules
Set regular times for going to bed and waking up. Consistency helps reset the internal body clock. Avoid large changes in sleep times, even on weekends. A steady schedule reduces nighttime wakefulness and daytime drowsiness. It also eases the “sundowning” effect, which causes agitation in the evening. Keeping a fixed sleep routine supports better rest and alertness during the day.
Daytime Activity And Light Exposure
Encourage physical activity during the day to promote tiredness at night. Activities like walking, gardening, or light exercise help maintain muscle strength and mood. Exposure to natural light, especially in the morning, resets the sleep-wake cycle. Open curtains or spend time outside for at least 30 minutes daily. Bright light exposure decreases sleep problems and reduces confusion.
Evening Relaxation Techniques
Create a calm atmosphere before bedtime to ease the transition to sleep. Gentle activities like reading aloud or listening to soft music help relax the mind. Avoid screens and bright lights, which can interfere with melatonin production. Keep the bedroom quiet and comfortably cool. These simple steps signal the body that it is time to rest.
Managing Daytime Sleepiness
Daytime sleepiness is common in dementia patients. It can affect their mood and daily routine. Managing this sleepiness helps improve overall wellbeing. Caregivers play a key role in balancing rest and activity.
Encouraging Engagement
Keeping dementia patients active reduces daytime sleepiness. Simple tasks like folding clothes or light gardening work well. Social activities like chatting or playing games help too. These activities keep the mind alert and body moving. Avoid long periods of inactivity during the day.
Balancing Rest And Activity
Short naps may benefit some patients but avoid long daytime sleep. Too much rest can worsen nighttime sleep problems. Schedule regular times for activity and rest each day. Encourage gentle exercise like walking to boost energy. Monitor their response and adjust the routine as needed.
Credit: www.aplaceformom.com
Medical And Therapeutic Approaches
Managing sleep issues in dementia patients requires a careful blend of medical and therapeutic approaches. Sleep problems can worsen cognitive symptoms and increase caregiver stress. Professional guidance helps identify the root causes and tailor treatments. Treatments range from medications to therapies that improve sleep quality without side effects.
Consulting Healthcare Professionals
Start by discussing sleep problems with a doctor or specialist. They can assess the patient’s overall health and dementia stage. Proper diagnosis is key to effective treatment. Healthcare providers may suggest sleep studies or blood tests to find underlying issues. Regular follow-ups help track progress and adjust care plans.
Medication Options
Doctors sometimes prescribe medicines to ease sleep difficulties. Common options include low-dose sedatives and melatonin supplements. These help regulate sleep cycles but require careful monitoring. Medication should be used only when benefits outweigh risks. Side effects and interactions with other drugs must be watched closely.
Non-pharmacological Therapies
Non-drug therapies play a vital role in managing sleep problems. Light therapy uses bright lights to reset the body’s internal clock. Relaxation techniques like gentle massage or calming music reduce anxiety and promote rest. Maintaining a consistent daily routine also supports better sleep patterns. These therapies often work well alongside medications.
Supporting Caregivers
Caregivers play a vital role in managing sleep problems in dementia patients. The challenges can be exhausting and stressful. Supporting caregivers helps improve care quality and their own well-being. Simple tools and resources make a big difference in handling nightly disruptions and agitation.
Understanding ways to cope, when to seek help, and how to build support eases the burden. It also promotes patience and resilience during difficult times.
Coping Strategies
Caregivers benefit from practical coping methods. Establishing a calm bedtime routine helps reduce agitation. Using soft lighting and soothing sounds can create a peaceful environment. Taking short breaks during the day allows caregivers to recharge. Keeping a sleep diary tracks patterns and triggers. Gentle exercise and fresh air during the day improve night sleep. Accepting help from others prevents burnout and stress.
Seeking Professional Help
Professional advice is key when sleep issues worsen. Doctors can assess underlying causes like pain or medication effects. Sleep specialists offer tailored treatments and tips. Therapists teach relaxation and stress management techniques. Support groups provide valuable emotional support and guidance. Early consultation avoids complications and improves sleep quality. Never hesitate to reach out for expert assistance.
Building A Support Network
Strong support networks ease caregiving challenges. Family members can share tasks and provide relief. Friends offer companionship and emotional encouragement. Community groups connect caregivers with similar experiences. Online forums share advice and resources. Local respite care services offer temporary breaks. A solid network reduces isolation and strengthens caregiver resilience. Together, caregivers can face sleep challenges more confidently.
Frequently Asked Questions
How To Keep A Person With Dementia In Bed At Night?
Create a calm bedtime routine with soothing music or reading. Keep the room dark, cool, and quiet. Limit daytime naps and encourage daily activity. Avoid screens before sleep. Consult a doctor for persistent sleep issues or medication options.
What Are Three Things To Never Do With Your Loved One With Dementia?
Never argue or correct them harshly, avoid overwhelming with too many questions, and never ignore their feelings or needs.
What Is The Number One Trigger For Dementia Behavior?
The number one trigger for dementia behavior is unmet needs, especially unrecognized physical or emotional discomfort.
What Stage Of Dementia Is Not Sleeping?
Sleep problems often start in the middle stage of dementia, worsening in the late stage. Nighttime restlessness and “sundowning” are common. Late stages may include reversed sleep-wake cycles, with more daytime sleep and nighttime wakefulness. Establishing routines and optimizing the sleep environment helps manage these issues.
Conclusion
Managing sleep issues in dementia patients requires patience and care. Creating a calm bedtime routine helps ease restlessness. A dark, quiet, and cool room supports better sleep. Encouraging daytime activity can reduce nighttime wakefulness. Watch for signs of discomfort or unmet needs.
Consult healthcare professionals for tailored advice and support. Small changes can improve sleep quality and daily life. Caregivers play a key role in providing comfort and stability. Consistency and understanding make a real difference every night.